Special Report: Personalised Medicine
2004-09-23: A number of separate announcements in recent days point to a growing interest in the area of personalised medicine among academic researchers and the pharmaceutical industry. Genetic treatments have already moved a significant distance from a theoretical concept to something which is being actively researched. The wider implications of the use of genetics for personalised medical treatment is also being considered.
On September 20, The Royal Society, the UK’s national academy of science, launched an investigation into the potential for designing drug treatments based on a person’s genetic makeup.
The study of how genetic factors influence a person’s response to a drug is known as Pharmacogenetics. It is seen as a way of making treatments as safe and effective as possible for every individual. (Most current drugs are not effective for 100 per cent of the population and some work in as few as 30 to 50 per cent of cases.) However, reservations have been expressed about the ability of this technology to fulfil such claims, what it might cost, how soon it could be achieved and if it would impact negatively on the modern healthcare system.
Sir David Weatherall, chair of the working group that will conduct the study, said: “Recent developments in understanding the biology and mechanisms of disease together with increased knowledge of genes have the potential to lead to major advances in healthcare over the next few decades. This study will look at whether pharmacogenetics, the designing of drug treatments based on a person’s genetic makeup, is a scientifically achievable aim, be it five, ten or 25 years from now. Equally importantly it will look at whether healthcare systems in the UK and elsewhere have the resources to implement such technologies and what the pharmaceutical industry’s assessment is of the significant investment needed to try and develop them in the first place.”
The Royal Society report will be published in summer 2005.
The use of genetics is not solely being researched from the point of view of curing illnesses. Sciona, Inc., a nutritional genomics company, based in New Haven, CT, USA, has recently announced the successful completion of a $4.1 million second round of financing to further develop products and markets for genetic personalisation of nutrition and personal care advice and products.
“There is a growing market in the U.S. for genetic personalisation amongst consumers, manufacturers and healthcare providers, as the link between disease and genetics has become better defined and validated. Individuals who are genetically predisposed to certain conditions or diseases may be able to mitigate onset or progression with personalised nutrition that matches their genetic profile,” explained Roger Wyse, Managing Director of Burrill & Company, a life sciences merchant which had a role in the financing arrangement. “As Sciona becomes established in the U.S. marketplace, the Company’s expertise in genetic personalisation and nutrition represents an enormous opportunity to influence this sector.”
Sciona develops tools and services that enable customers to customise personal care and nutrition products based upon an individual’s genetic profile. Through both acquisition and development, Sciona has created a portfolio of patent applications surrounding its proprietary method of providing personalised lifestyle advice based on analyzing individuals’ DNA for specific genetic variation and taking into consideration environmental and lifestyle factors. Currently, Sciona has two products on the market in the U.S. and Europe for DNA testing and automated interpretation of those tests. To date, over 4,500 consumers in the U.S. and Europe have purchased genetically personalised products or services from channel partners that utilize Sciona’s technology and services. Sciona collaborates with Genaissance Pharmaceuticals in the U.S. to conduct genetic testing, as well as studies to prove the efficacy of novel active ingredients in nutrition and personal care products.
“Closing on this round of financing is an important milestone, as the funding enables us to expand geographically and focus on the U.S. marketplace,” said Chris Martin, President and Chief Executive Officer of Sciona. “We are pleased to have such a strong international syndicate of investors, and with their backing plan to build on our leading position in nutrition genetic research and identify new partners with whom to bring our products to market.”
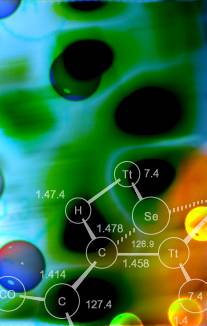
In addition to its use in treatment and nutrition, genetic profiling has also been applied to the area of diagnostics. The Diagnostics division of Roche, the Swiss pharmaceutical giant, has announced that its AmpliChip CYP450 Test, which analyses variations in two genes that play a major role in the metabolism of many widely prescribed drugs, now has the CE mark ("Conformité Européene") This allows the test to be used for diagnostic purposes in the European Union. The test detects genetic variations in the Cytochrome P450 2D6 and 2C19 genes, and provides the associated predictive phenotype (poor, intermediate, extensive, or ultra-rapid metabolizer). Results can be used by physicians as an aid for selecting drugs and individualizing treatment doses for drugs primarily metabolized by the enzymes these genes encode.

The Roche Diagnostics AmpliChip CYP450 Test
"This specific test is the first representative of an exciting new technology which holds great potential for diagnostic applications," said Heino von Prondzynski, Head of Roche Diagnostics and Member of the Roche Executive Committee. "With the CE mark for the AmpliChip CYP450 Test, we are on our way to helping physicians move toward a more personalised approach to therapy, and to building our new line of chip-based diagnostics products."
The AmpliChip CYP450 Test uses two industry gold-standards, Roche polymerase chain reaction (PCR) amplification technology and Affymetrix high-density microarray technology (glass chips arrayed with tens of thousands of DNA fragments yet no bigger than a thumbnail). Affymetrix announced that its GeneChip® System 3000Dx instrumentation, on which the AmpliChip CYP450 Test is run, is now also CE marked and available for diagnostic use in the European Union.
Enzymes encoded by the CYP2D6 gene metabolize many anti-depressants, anti-psychotics, anti-arrhythmics, pain drugs, anti-emetics, and beta-blockers (beta-adrenergic receptor blocker drugs). Enzymes encoded by the CYP2C19 gene metabolizes drugs from a variety of classes, including anti-convulsants, proton pump inhibitors, anti-coagulants, benzodiazepines, and anti-malarials.
Poor metabolizers treated with drugs that are extensively dependent on certain "normal" enzyme activity are at increased risk for excessive or prolonged levels of the drug in their blood (excessive or prolonged therapeutic effect) and toxicity, while ultra-rapid metabolizers may not achieve sufficient therapeutic levels in their blood with standard dosing. In the case of pro-drugs (these are drugs that require enzymatic action before they become the therapeutic compound in the body), the opposite phenomenon occurs. In addition, drugs taken at the same time (concurrent medications) and other environmental factors such as diet can inhibit or induce Cytochrome P450 enzyme activity.
To allow highly accurate prediction of patient phenotype, the AmpliChip CYP450 Test has the ability to detect not just the presence of CYP2D6 gene duplications, but also to discern which variation of the gene (allele) has been duplicated. This specificity is important in correctly predicting the ultra-rapid metabolizer phenotype and avoiding potential mis-classification of the patients tested.
These rapid developments in genetics-based medicine present a set of ethical and legal questions which have not yet been fully addressed. One organisation which has examined this topic is the Centre for Technology Assessment (TA-SWISS). TA-Swiss has the objective of transmitting independent information on the potential, the risks, and the repercussions of new technologies. They have investigated the opportunities and risks inherent in the current developments in
pharmacogenomics and pharmacogenetics.
The growing number of biobanks is one area that, in the view of the authors, requires special attention. The laws covering human research and genetic testing on human beings will make it possible for politicians with
foresight to establish “crash barriers” for the emerging developments in pharmaceutical research. The TA-SWISS study provides some impetus in this regard. Different patients may react in different ways to the same drug: in many people a particular
therapeutic product will have the expected effect, in some people there is no effect at all, and a few
people may experience side-effects – in some cases serious ones. Such differences may have a
genetic cause, as there are minimal differences in our individual genotypes. While pharmacogenetics is
concerned with the improved safety and efficacy of pharmaceutical products, the broader field of
pharmacogenomics, by contrast, seeks out strategies for improving pharmaceutical development.
The report says that metaphors such as “personalised
medicine”, “designer drugs” and “personal pills” that are often encountered in texts on
pharmacogenetics and pharmacogenomics are misleading. These metaphors cause expectations to
be set too high, and actually obscure the true potential, namely the development of new drugs that
can be used more selectively and with fewer side-effects. “In the future we will still be buying our
drugs off the peg”, stresses Klaus-Peter Rippe, Project Manager of the TA-SWISS Study. But Rippe
goes on to say that developments are moving towards a splitting up of the population into different
genetic sub-groups, which could then be administered the drug most suitable for them in each case.
In very rare cases, one genetic variant is solely responsible for the occurrence of a disease or for the
success of a drug therapy. As described above in relation to Siona, Inc., genome research is increasingly focusing on the functions of genes and
their role in the interplay with environmental factors and lifestyles. To be able to investigate the
complex interactions, it is necessary to gather large quantities of genetic and lifestyle data. For this
purpose, what are known as “biobanks” are being set up to hold thousands of blood and tissue
samples. These will be used to examine genetic factors, a central element of genome-based
therapies. The authors of the TA-SWISS study have identified a need for statutory regulation, and
recommend strict data protection law provisions and as far as possible decentralised forms of
organisation and pseudonymisation of samples. Concomitant research should subsequently consider
the ethical, legal and social aspects of biobanks, and there should be greater data security in the
academic sector.
The TA-SWISS study states that pharmacogenetics and pharmacogenomics do not, as is commonly asserted, have a clearly defined
potential for discrimination. It is certainly true that pharmacogenetic approaches can identify patients
for whom a specific drug would have no effect, or would cause serious side-effects. But it is wrong to
infer from this that these groups would unjustifiably be treated differently. With regard to health
insurance, it is important to distinguish between compulsory basic insurance and supplementary
insurance. In Switzerland's basic insurance system, which is set up according to the principle of solidarity, discrimination based on pharmacogenetic information may be virtually excluded - provided the right to be accepted for insurance irrespective of health risks remains in the future, and compulsory basic insurance is not undermined in terms of its benefits.
The potential significance of pharmacogenetic and pharmacogenomic testing is not immediately or
conclusively obvious. For that reason, the authors of the TA-SWISS study recommend that the law
should not permit any reduced level of protection for genetic data in the field of pharmacogenetics. Indeed, the handling of so-called “surplus information”, i.e. statements on a person’s predisposition to
certain diseases that were not actually the object of the investigation, is something that has yet to be
regulated in Switzerland. Statutory “crash barriers” could be laid down in laws on human research or on genetic tests carried out
on human beings. Because of the foreseeable development of pharmacogenomics, the handling of
pharmaceutical products for rare diseases with small patient groups, and correspondingly small markets (so-called “orphan drugs”) should be given much greater prominence in the law than has
been the case up to now. Finally, the TA-SWISS study recommends, in addition to intensified training and further training for doctors, that there should be a broader public debate on the central questions
raised relating to health policy.
The question of protecting the privacy of patients' genetic data has not been neglected among researchers. A recent development (previously reported in MadeForOne.com) is a new technology developed by scientists at IBM, that could bring the promise of personalised medicine one step closer to reality.
Using a basic computer language, the researchers created a "smart" DNA stream that contains a patient's entire medical record, according to a report in the upcoming Oct. 11 print edition of the Journal of Proteome Research, a peer-reviewed journal of the American Chemical Society, the world's largest scientific society. (The report was published online July 22.)
To achieve the potential of genetic medicine, scientists need a way to store and efficiently transmit whole sequences of patient DNA with built-in privacy -- a hurdle that has yet to be overcome, according to the authors of the report.
IBM's Genomic Messaging System (GMS) provides a basic computer language that can be inserted into DNA sequences to bridge the gap between patient medical records and genetic information, says lead author of the paper, Barry Robson, Ph.D., a chemist at IBM's T. J. Watson Research Center in Yorktown Heights, New York.
The stream of information transmitted is basically a "smart" DNA sequence containing a patient's entire medical record in compressed form as well as genetic information. "It is a stream of DNA symbols -- GATTACAGATTACA -- with GMS language inserted at appropriate points," Robson says. The inserted language can be used to annotate the DNA, to link to relevant medical data, and to control the privacy of selected sequences with passwords, among others.
"GMS links archives of digital patient records to enable analysis of those records by a variety of bioinformatic and computational biology tools," says Robson. These tools include data mining to discover unexpected relationships, large-scale epidemiological studies and three-dimensional modeling of patient proteins to study the effect of "SNiPs" -- single nucleotide polymorphisms.
Scattered throughout the human genome are millions of one-letter variations in genetic code known as SNiPs. Most are harmless, but some SNiPs provide crucial information, because they can help pinpoint the location of genes that might influence certain diseases.
GMS also provides platforms for respecting the privacy and security of a patient, including a flexible system of passwords that releases only selected parts of the patient's DNA sequences to different researchers. And since future applications might include medical emergencies, the system has been designed to continue operation even in the event of a disaster by providing a transient backup.
In addition to the technical barriers, there are considerable challenges to be resolved in devising a legal framework for personalised medicine. A further difficulty for the world at large is that advances in personalised medicine in wealthy nations may be denied to developing countries due to costs and information system requirements. Even in developed nations with less than perfect health systems, those on low incomes could find themselves relegated to a second division of healthcare, while the most advanced personalised treatments are offered to those who can afford them. There is no doubt that a complex journey is ahead for the development of personalised medicine.
|
